advertisement

Glaucoma Dialogue IGR 20-4
Comment

Comment by Michele C. Lim on:
82885 Review of hygiene and disinfection Recommendations for outpatient glaucoma care: A COVID era update, Shabto JM; De Moraes CG; Cioffi GA et al., Journal of Glaucoma, 2020; 29: 409-416
See also comment(s) by Ningli Wang & Chunyan Qiao • Luciano Quaranta • Poemen Chan & Clement Tham • Brandon J. Wong • Tin Aung & Rahat Husain • Pradeep Ramulu • Andrew Camp • Clement Tham & Poemen Chan •Shabto and colleagues write an excellent summary of recommendations for hygiene and disinfection for outpatient glaucoma care in the COVID-19 era. So much has changed in our approach to the delivery of health care since the emergence of SARS-CoV-2 (Severe acute respiratory syndrome coronavirus 2) and this is a timely compilation of practical recommendations for any eye care practice. Many of the cleaning recommendations are easy to follow and most practices are well-versed in the disinfection of tonometer tips and of contact laser lenses but there are two items that are particularly challenging. One, how to clean the bowl of a visual field device and two, the practical implications of cleaning handheld lenses.
The recommendations for cleaning the bowl of the Octopus 900 perimeter and Humphrey visual field analyzers are different. Haag-Streit Diagnostics warns that the bowl of the Octopus is lined with a special paint that could be damaged with detergents but recommends wiping any residue with a soft cloth and soap-suds but they do not offer any evidence that this will eliminate SARS-CoV-2.1 Carl Zeiss Meditech, Inc. provides updated information in which the bowl should be sprayed lightly with 70% Isopropyl solution should it become contaminated with respiratory droplets.2 In our practice, to further protect against contamination, we have created an acrylic shield that creates a wall between the patient and perimeter bowl (Fig. 1).
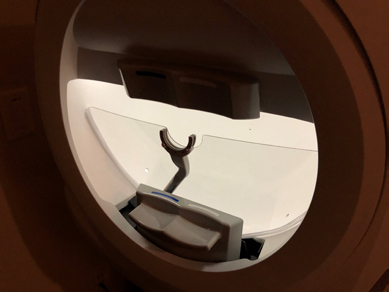
Fig. 1. Acrylic breath shield designed for an automated visual field machine.
Now that patients wear masks to their visit, I notice that the condensation from their breath shoots upwards and may collect on my handheld lens and hand and Shabto and colleagues offer excellent recommendations for lens cleaning. But to do so, we must have duplicates in order to rotate lenses between patients and for large institutions this comes with a large cost. If I soak them in Cidex or hydrogen peroxide, is there a safe location near the exam rooms where patients or children can't access the cleaning solutions? Is it practical to use disposable lenses? Volk sells a disposable 28D handheld lens but at a cost of $14.50 per lens! Would UV light cleaning devices work well to disinfect handheld lenses? In our clinic, we use a UV light disinfection unit (which was intended for CPAP gear) (Fig. 2) to clean handheld lenses and it requires a short 5-minute cleaning cycle. Some studies suggest that one can eliminate SARS-CoV-2 with this methodology.3,4

Fig. 2. Ultraviolet light sterilizer.
Since the initial writing of this article, the United States is now in a period of health care restoration and this means the volume of patients will rise in the coming months making it even more essential to understand how to protect both patients and staff from SARS-CoV-2 exposure. The CDC issued recommendations to aid health care organizations in restoring routine patient care and they provide a "Framework for Healthcare Systems Providing Non-COVID-19 Clinical Care During the COVID-19 Pandemic.5 Restoring health care in our busy ophthalmology practices will require unique solutions to maintain physical distance between patients once the volume of visits begins to 'ramp up'. At the UC Davis Eye Center, we began reinstating routine patient visits on 5/4/2020 and are currently scheduling at 50% volume to ensure that we can maintain proper patient physical distancing. We allow one person to accompany a patient if needed and we have employed restaurant-style 'pagers/buzzers' to allow patients to wait in their car or elsewhere so as not to overload waiting rooms. We have created a Saturday imaging (OCT, fundus photos, slit lamp photos) and procedures (visual fields) clinic to decompress the Monday to Friday work week. This Saturday clinic also helps sustain video visits. Video visits have been a challenge to ophthalmology because of its inability to capture the details of an eye exam. We are embarking on a workflow in which patients who come for Saturday imaging or procedures may also have their vision and intraocular pressure measured by technical staff. This can then be followed by a video visit with the physician to discuss diagnoses and treatment plans. Separating the physician-patient visit from imaging/procedures can help decrease the amount of time patients spend in the office. We have also piloted drive-up visits (Fig. 3) in which vision and pressure are checked while the patient remains in their car and this is followed by a video visit with the physician. As we look to the future, most of us realize that life will never be the same again, at least until a SARS-CoV-2 vaccine is created, and we must continue to employ out-of-the-box ideas to sustain our practices.
References
- Octopus Perimeters. Considerations on how to clean perimeters to lower the risk of COVID 19 transmissions. Haag-Streit Diagnostics Website (https://www. haag-streit.com/fileadmin/Haag-Streit_Diagnostics/_ALLGEMEINE_BILDER_ UND_ICONS/Corona/PDFs/2020-03-26_Desinfection_of_Perimeters_FINAL.pdf) Published 2020. Accessed May 13, 2020.
- Cleaning Guidance for the Humphrey Field Analyzer (HFA). Carl Zeiss Meditech, Inc Web site. . ((https://www.zeiss.com/meditec/int/med-support-now/disinfectingophthalmic- devices.html) Published 2020. Accessed May 13, 2020.
- Kolata G. As Coronavirus Looms, Mask Shortage Gives Rise to Promising Approach. New York Times. https://www.nytimes.com/2020/03/20/health/coronavirus-masksreuse. html?searchResultPosition=1. Published 2020. Accessed May 14, 2020. Fig. 3. Drive-up glaucoma visit with intraocular pressure measurement.
- Narla S, Lyons AB, Kohli I, et al. The importance of the minimum dosage necessary for UVC decontamination of N95 respirators during the COVID-19 pandemic. Photodermatol Photoimmunol Photomed 2020.
- Framework for Healthcare Systems Providing Non-COVID-19 Clinical Care During the COVID-19 Pandemic. Centers for Disease Control and Prevention Web site. https://www.cdc.gov/coronavirus/2019-ncov/hcp/framework-non-COVID-care. html. Published 2020. Accessed May 13. 2020.
Comments
The comment section on the IGR website is restricted to WGA#One members only. Please log-in through your WGA#One account to continue.Log-in through WGA#One

