advertisement

Editors Selection IGR 21-4
Basic Science: Corneal effects of prostaglandins

Comment by Cynthia Roberts on:
78821 Experimental Evaluation of Travoprost-Induced Changes in Biomechanical Behavior of Ex-Vivo Rabbit Corneas, Zheng X; Wang Y; Zhao Y et al., Current Eye Research, 2018; 0: 1-6
This is a critically important study for any clinician in measuring intraocular pressure (IOP) while treating patients with prostaglandins analogs (PGA). IOP is the load that generates stress on the cornea. It can easily be seen in Figure 3 that as IOP and the associated stress increases, the elastic modulus (tangent slope) also increases and the cornea exhibits stiffer behavior at higher IOP. Therefore, it is quite difficult to separate the effect of lowering IOP with PGA treatment from the effect on the intrinsic corneal properties, when both reduce the stiffness response. This study removes the confounding effect of IOP and focuses strictly on the change in the material properties of the cornea in a well-conducted, careful investigation.
From a clinical perspective, the pre-treatment cornea would be at a point on the control group curve with open circles on the left in Figure 3 (see the original article) at a specific IOP. Post-treatment, the cornea would move down the curve as IOP is lowered, and also jump to the curve on right due to the change in corneal properties. This has a profound effect on any tonometer technology that is affected by corneal properties, including Goldmann Applanation tonometry (GAT),1 the most common tonometer in the world. In other words, GAT underestimates the IOP with PGA treatment, and overestimates the amount of lOP lowering that has occurred.
Clarification of the clinically available biomechanical parameters is offered, including corneal hysteresis (CH) and corneal resistance factor (CRF) from the Ocular Response Analyzer, as well as deformation amplitude (DA) from the Corvis ST. The authors state that CRF is a measure of corneal stiffness, which is not completely accurate. CRF is an empirically derived parameter designed for maximum correlation with central corneal thickness (CCT). However, it is a function of both the loading and unloading applanation pressures, so it is also influenced by viscoelasticity. Unlike CH which is a simple difference between the two applanation pressures, CRF is weighted more heavily by the loading applanation pressure so it has a stronger relationship to the elastic response. Fundamentally, though, it remains a viscoelastic parameter. In addition, the authors state that DA is a measure of corneal stiffness, which is a bit misleading. The strongest influence on DA is IOP, with corneal stiffness having a much smaller influence than IOP. The paper referenced2 did not show a reduction in DA with PGA treatment, but was a cross-sectional study comparing long-term PGA use against both normal controls and newly diagnosed glaucoma. They did not study the response to newly-initiated PGA treatment. In addition, the authors cited inconsistent results with regard to CH after PGA treatment. The only cited paper3 that showed a decrease in CH was not a study of prostaglandin naive subjects, but a cessation of PGA treatment where corneal biomechanical effects had already occurred. Other papers cited showed an increase in CH with initial prostaglandin treatment, combined with a reduction in IOP, and were consistent in reported response.
GAT underestimates the IOP with PGA treatment, and overestimates the amount of lOP lowering that has occurred
An example of the artifact produced using GAT in combination with PGA treatment is with a patient seen in The Ohio State University clinic with GAT of 11 mmHg in both eyes after treatment with PGA's. Yet, the left eye had rapidly progressive visual field loss and the right eye was stable. However, when measured with other technologies including the PASCAL Dynamic Contour Tonometer (OD: 16.0 mmHg; OS: 17.5 mmHg), both eyes had higher pressure than measured with GAT and the IOP in the left eye was greater than the IOP in the right eye, consistent with the field loss. The Corvis ST confirmed visually the left eye had greater IOP than the right eye, as shown in the overlapped deformation images of both eyes in Figure 1. The deformation amplitude in the left eye was visibly less than in the right eye, which means the left eye had greater resistance to deformation with higher pressure than the right. This was not recognized by GAT. Figure 2 shows the associated visual fields.4
It is important for glaucoma specialists to ask themselves if IOP is an appropriate target when using PGA's for treatment, or in comparing IOP-lowering medications in clinical trials. If PGAs reduce IOP as well as induce artifact which causes underestimation of IOP due to a reduction in corneal stiffness, comparisons with other medications are confounded. At best, a tonometer technology other than applanation, including GAT, should be used to estimate IOP if PGAs are used for treatment or in clinical trials.
 Fig. 1. Overlapped single frames extracted from Corvis ST videos from the left eye, pseudo-colored red, and the right eye, pseudocolored blue, both at highest concavity or maximum displacement. The smaller displacement of the left eye means the IOP is higher than the right, consistent with visual fields in Figure 2.
Fig. 1. Overlapped single frames extracted from Corvis ST videos from the left eye, pseudo-colored red, and the right eye, pseudocolored blue, both at highest concavity or maximum displacement. The smaller displacement of the left eye means the IOP is higher than the right, consistent with visual fields in Figure 2.
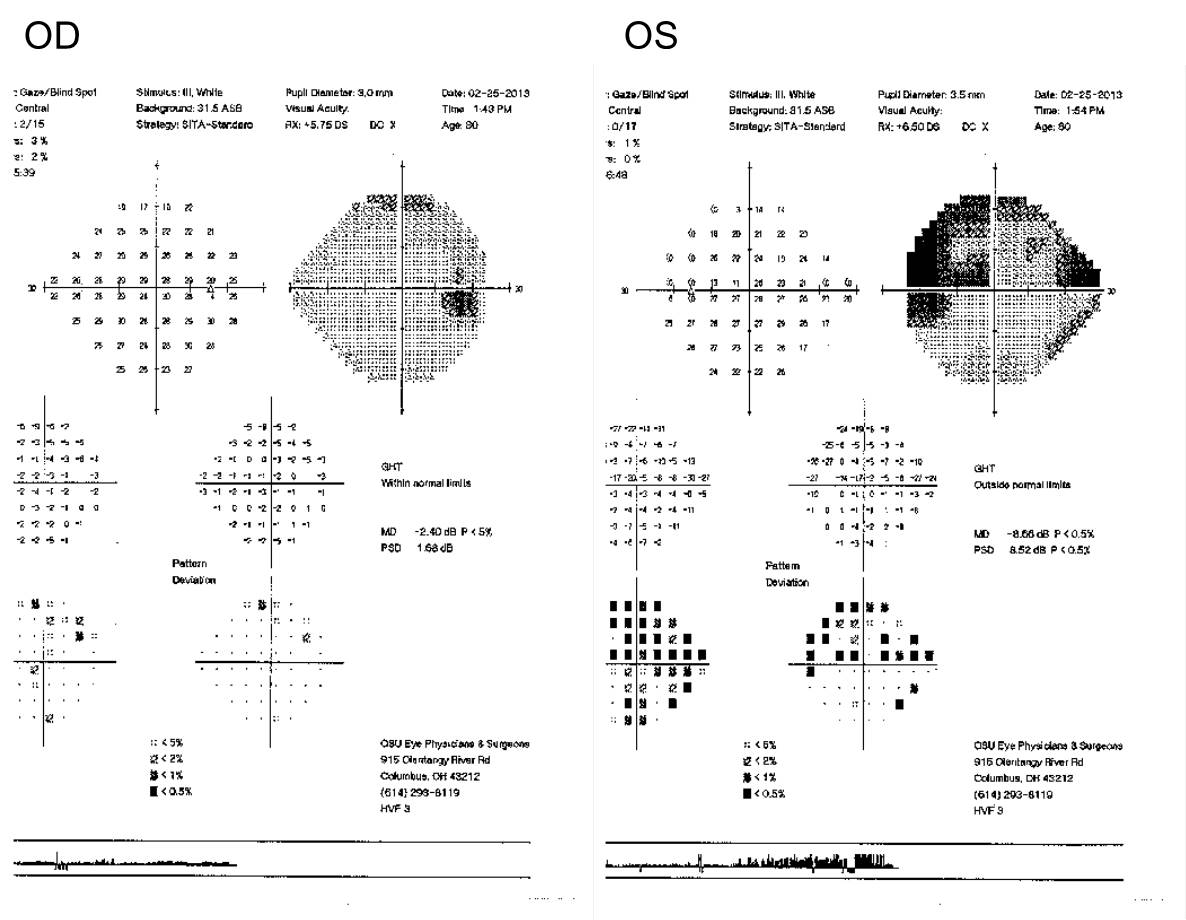 Fig. 2. Visual fields of patient shown in Figure 1.
Fig. 2. Visual fields of patient shown in Figure 1.
References
- Liu J, Roberts CJ. Influence of corneal biomechanical properties on intraocular pressure measurement: Quantitative analysis. J Cataract Refract Surg 2005;31(1):146-155.
- Wu N, Chen Y, Yu X, et al. Changes in corneal biomechanical properties after longterm topical prostaglandin therapy. PLoS One. 2016,11,e0155527.
- Meda R, Wang Q, Paoloni D, Harasymowycz P, Brunette I. The impact of chronic use of prostaglandin analogues on the biomechanical properties of the cornea in patients with primary open angle glaucoma. Br J Ophthalmol 2017;101:120-125.
- Weber PA, Johnson RD, Sawchyn A, Mahmoud AM, Roberts CJ. Intra-ocular pressure measurement in asymmetric glaucoma. American Glaucoma Society, New York, March 2012.
Comments
The comment section on the IGR website is restricted to WGA#One members only. Please log-in through your WGA#One account to continue.Log-in through WGA#One

