advertisement

Editors Selection IGR 7-1
Progression: A system to measure and classify RNFL progression

Comment by Anja Tuulonen on:
26260 Patterns of progression of localized retinal nerve fibre layer defect on red-free fundus photographs in normal-tension glaucoma, Suh MH; Kim DM; Kim YK et al., Eye, 2010; 24: 857-863
Suh et al. (768) report a system to measure and classify progression of retinal nerve fiber layer (RNFL) defects in 65 patients selected to the study because of RNFL progression. The concomitance of RNFL progression to progressive visual field (VF) and optic disc changes is shown in the Table and compared to the EMGT and OHTS indicating how selection affects the huge distributions what gets detected. The significance of short follow-up window is also emphasized in the paper of Suh et al. who discuss that short follow-up period of six months after RNFL progression may explain the poor correlation between RNFL and VF.
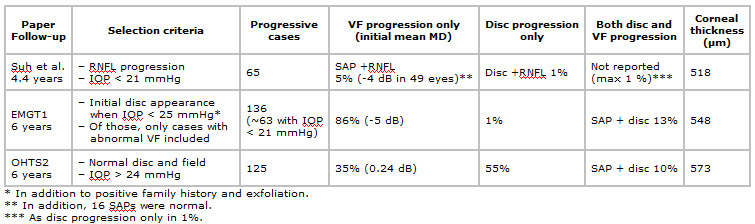
Concomitance of RNFL, optic disc and visual field progression in different studies. The results indicate how selection criteria affect the huge distributions what gets detected and support the statement of a systematic review 'Nerve fibre layer, optic disc and visual field changes manifest themselves at different times during the follow-up period (usually with a delay of one to six years) and their correlation at any given time-point is poor'3. The seeming discordance probably reflects just the short length of the follow-up window of the studies compared to natural history of glaucoma.
Suh et al. nicely describe the large individual variability in RNFL progression seen in every clinic: development of new defects together with widening and 'deepening' (= better visibility) of the existing defects as well as optic disc hemorrhage appearing at the border of normal and abnormal RNFL, foretelling future direction of progression. In addition to confirming that RNFL imaging is helpful during followup, the main value of the paper is to describe a reproducible method (k values ≥ 0.79) to measure RNFL defects and their progression in scientific papers. While such measurements are not practical in every-day practice, the 'deepening' of the defect may be detected easier by evaluation the visibility of the RNFL defect extending towards disc margin (not mentioned in Suh et al.'s paper). Widening of existing defect may be easier to detect comparing its border to the small retinal vessels than at the disc margin.
References
- Heijl A, Leske MC, Bengtsson B, Hyman L, Bengtsson B, Hussein M & the EMGT Group (2002): Reduction of intraocular pressure and glaucoma progression. Results from the Early Manifest Glaucoma Trial. Arch Ophthalmol 120: 1268-1279.
- Kass MA, Heuer DK, Higginbotham EJ et al (2002): The Ocular Hypertension Treatment Study. A randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol 120: 710-713.
- Tuulonen A,. Airaksinen PJ, Erola E, Forsman E, Friberg K, Kaila M, Klemetti A, Oskala P, Puska P, Suoranta L, Teir H, Uusitalo H, Vainio-Jylha E,. Vuori M-L. The Finnish evidence-basedguideline for open-angle glaucoma. Acta Ophthalmol. Scand. 2003: 81: 3-18
Comments
The comment section on the IGR website is restricted to WGA#One members only. Please log-in through your WGA#One account to continue.Log-in through WGA#One

