advertisement


What Does the Sclera Have to Do With Glaucoma?
C. Ross Ethier, Ian A. Sigal and John G. Flanagan
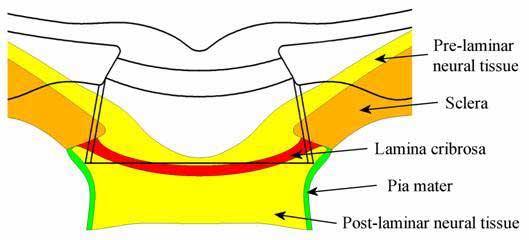
It has long been hypothesized that biomechanical effects might play a
role in glaucomatous optic neuropathy, as elevated IOP induces stretching
and deformation in the optic nerve head. Recently, engineering modelling
techniques have been used to determine how the optic nerve responds to acute
changes in pressure (see e.g. IOVS 45: 4378 and 45: 4388, 2004).
The models make some intriguing predictions, one of which is that the
biomechanics of the corneo-scleral shell affect the optic nerve head quite
profoundly. Why? It has to do with effective stiffness: the
thick, solid sclera is much stiffer than both neural tissue and the porous
lamina cribrosa. It's as if a wire rope (the sclera) were attached to a
thick elastic band (the lamina cribrosa); if you pull on the wire rope,
the elastic simply has to follow. The implication is that acute deformations
of the lamina cribrosa and neural tissue depend critically on how much the
sclera deforms, and hence on the mechanical properties of the sclera. As
the image below shows, and as seen in more detail in the movie available
on the journal web site, the resulting deformations of optic nerve tissues
are substantial.
What does this mean? It suggests that the properties of the corneo-scleral
shell, and especially the peripapillary sclera, can influence how much mechanical
insult is experienced by retinal ganglion cells and optic nerve head glia.
These model predictions need experimental confirmation, but we wonder whether
this might explain some of the association between central corneal thickness
and progression seen in the OHTS study, even after correction of corneal
thickness-compensated IOP.
Click on figure for a dynamic view
Predicted deformations of optic nerve tissues as IOP goes from 15 to 50 mmHg. Black lines represent the configuration at low pressure; coloured regions are the corresponding high pressure configuration. Note that deformations have been exaggerated 6-fold to facilitate visualization.