advertisement

Scientific photos
Optic nerve macrophages
Jelena Kezic and Jonathan Crowston
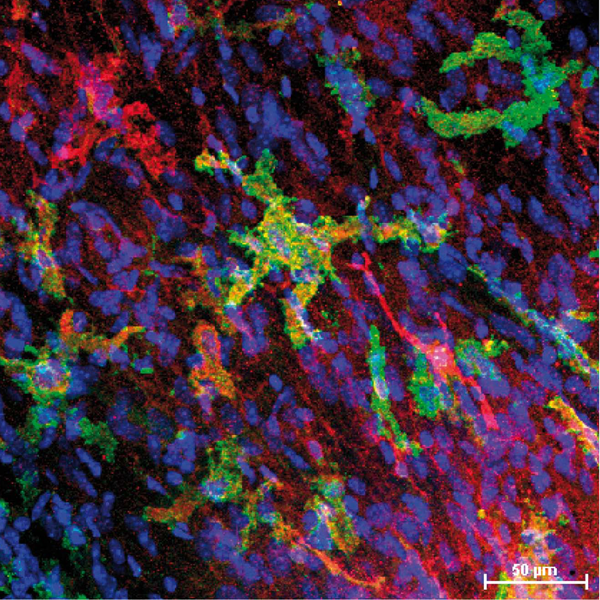
Confocal microscopic image showing the resident macrophage population in the optic nerve of a 12-month old C57BL/6 mouse. Immuno-fluorescence staining of optic nerve whole-mount preparations were performed using the macrophage markers anti-Iba-1 (ionized calcium binding adaptor molecule 1; shown in red), and anti-H2-I-A/I-E (M5/114; MHC Class II; shown in green). Nuclei were stained using DAPI (shown in blue). Images were taken at 40X magnification.
Jelena Kezic and Professor Jonathan G. Crowston
Centre for Eye Research
Australia, University of Melbourne
32 Gisborne Street
East Melbourne
VIC 3002
Australia
Retinal ischemia-reperfusion-induced early onset macroglial and microglial responses in the retina and optic nerve head
NingLi Wang*, ShaoDan Zhang and Qingjun Lu
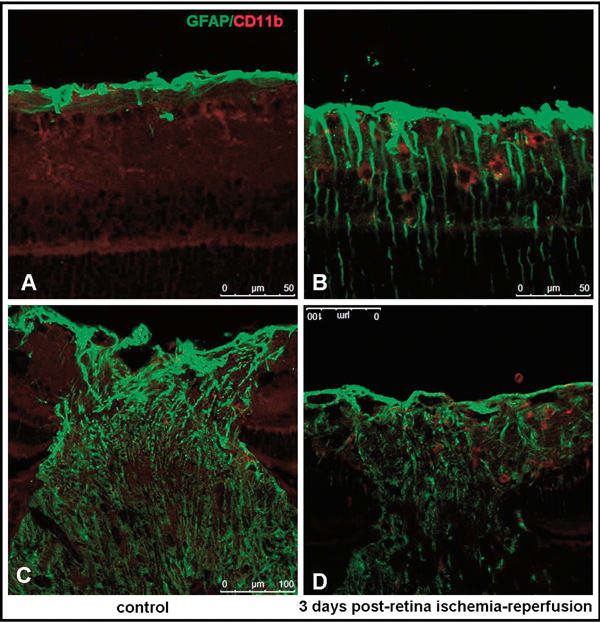
To demonstrate the response of glial cells in the retina and optic nerve head (ONH) in a rat model of transient intraocular hypertension, or so called retinal ischemia-reperfusion, GFAP and CD11b were used as markers for astrocytes and microglia, respectively. In control rats, GFAP-positive signals were confined to the nerve fiber layer (NFL) and ganglion cell layers (GCL) in the retina. Only processes-like immunolabelling of CD11b without identifiable cell body were observed scattering in the inner plexiform layers (IPL) and GCL. In ONH, longitudinally arranged GFAP-labeled processes run across the ONH into optic nerve. Few CD11b-positive microglia with ramified morphology were observed. Three days after retinal ischemia-reperfusion, an obvious increase in GFAP immunoreactivity in the retina was noticed. Intensely stained GFAP processes extended across the entire thickness of the retina. The number of CD11b immunoreactive microglia increased dramatically. These cells showed amoeboid-like cell bodies and shortened and thick processes with little branches. Architecture of the GFAP-positive processes in the ONH became irregular. A large amount of activated microglia were also observed in this region. These findings suggest that both macroglia and microglia may be involved in the initiation and progression of glaucomatous RGCs loss and axon injury, which may associated with the mechanisms of inflammation and immunity.
* Correspondence to Professor Ningli Wang, Beijing Tongren Eye Center, Capital Medical University Affiliated Beijing Tongren Hospital; Beijing Ophthalmology & Visual Science Key Lab,Beijing China, 100730.E-mail: wningli@163.vip.com

