advertisement


Reflections from the nerve fiber layer in glaucoma
October 10-14, 2001, New Orleans, LA, USA
Robert N. Weinreb
The Robert N. Shaffer Lecture at the 105th Annual Meeting of the American Academy of Ophthalmology delivered by Robert N. Weinreb, who described the rationale for examining the retinal nerve fiber layer, reviewed conventional diagnostic methods, and discussed innovative technology to improve the examination
An early edition of the Becker Shaffer textbook, Diagnosis and Therapy of the Glaucomas, stated that, for examination of the retinal nerve fiber layer, "there are sporadic encouraging reports of its value in glaucoma". This statement was prophetic, and a considerable number of studies have subsequently validated the use of retinal nerve fiber layer examination for both diagnosing and monitoring the progression of glaucoma. Retinal nerve fiber layer defects are found in almost 90% of ocular hypertensive eyes at the time visual field loss first occurs, and many eyes already have retinal nerve fiber layer defects several years before field loss. Common errors with ophthalmoscopic assessment of the retinal nerve fiber layer and in interpreting retinal nerve fiber layer photographs include overestimation of focal retinal nerve fiber layer defects and underestimation of mild diffuse atrophy. With focal defects, it is important to consider the width and pattern. With diffuse atrophy, the clarity of vessels should be considered and compared with the contralateral eye. Even with the most experienced observers, the retinal nerve fiber layer is poorly visualized with conventional testing techniques in the presence of a miotic pupil, cataract, or lightly pigmented fundus.
An array of innovative instruments were discussed that have been developed to reduce the subjectivity of retinal nerve fiber layer examination. Each of the instruments relies on different properties of the retina to measure and provide large amounts of descriptive information. Compared with the ophthalmoscopic or photographic examination, these instruments provide data that are objective, quantitative, highly reproducible, and do not require laborious processing.
- Confocal scanning laser ophthalmoscopy measures the intensity of reflected light from the retinal surface in order to calculate topographic measurements. It is most appropriately used for assessing optic disc topography, and not for evaluating the thickness of the retinal nerve fiber layer.
- Optical coherence tomography measures the echo time delay of light backscattered from different layers in the retina, using low-coherence interferometry. A new version of the instrument, the OCT 3, allows as many as 512 points to be evaluated, a marked increase over earlier versions of the instrument.
- Scanning laser polarimetry measures retardation, the change in polarization of incident light due to the birefringent properties of the retinal nerve fiber layer. More than one-third of patients assessed with a commercially-available instrument have had inaccurate measurements due to the use of an assumed fixed compensation for anterior segment changes. These appear to have been resolved with modification of the instrument to individually compensate and correct for anterior segment birefringence.
Each of these techniques has specific advantages and disadvantages. One technique has not been found best for all purposes, or for all patients. In conclusion: "It is likely that the best technique will depend on specific clinical needs, patient population, and how the technology continues to evolve."
Structure Function in Glaucoma
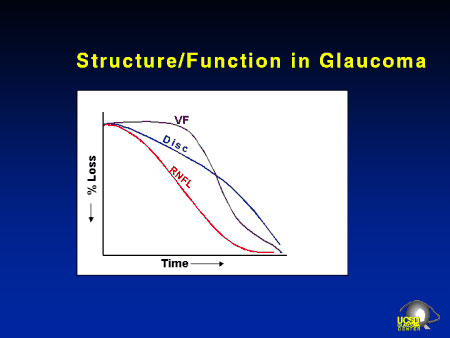
Hypothesized rate of retinal nerve fiber layer, optic disc, and visual field changes in glaucoma. Rates of changes likely depend on individual patients.

